Who's Afraid of a PSA?
By Ralph Blum
The straight answer? Every guy who’s ever been told his PSA was elevated for his age, and that he needs to have a biopsy. Because from that point on, things can happen fast. It’s the prostate cancer version of baseball’s famous Tinker-to-Evers-to-Chance double play—PSA Test-to-Biopsy-to-Surgery.
The PSA is a simple blood test for prostate-specific antigen, a protein produced by normal prostate cells. Cancer cells, however, produce more PSA per unit volume than benign cells, so an elevated PSA can be cause for concern. Since 1986, PSA testing, although not perfect, has served as the gold standard for widespread screening and early diagnosis of prostate cancer. Controversy arises from the fact that, at the first sign of an elevated PSA, your family doctor is likely to send you to a urologist who will almost certainly perform a biopsy—all too often opening the door to unnecessary radical treatment.
Avoiding False Readings
There are other factors besides prostate cancer that can influence PSA test results. Here are some of them:
BPH: Benign prostatic hyperplasia, prostate enlargement caused by age or infection, induces an elevated PSA not indicative of cancer.
Infection: Consider the possibility of infection. Some years ago, when my PSA spiked unaccountably from 7.4 to 20.3, my wife, Jeanne, who is a medical intuitive and practices Traditional Oriental Medicine, suggested to our family doctor that he put me on a course of the antibiotic Cipro. Which he did, and after ten days my PSA had dropped back to 9.25.
The 48 Hour Rule: It is possible that strenuous exercise, heavy lifting (like lugging suitcases through airports), sexual activity, and even bicycle riding before a PSA test will negatively effect the result. However, a false elevation is guaranteed if you get your PSA checked immediately following a Digital Rectal Exam (DRE) or too soon after intercourse. So don’t have a blood test for at least a week after a DRE, and avoid ejaculation for 48 hours before the test.
Inconsistent Lab Work: Standardization of tests, or assays, from one lab to another, is still lacking. This makes comparisons between PSA tests done in different labs unreliable. If you have two or more PSA tests, make sure they go to the same lab for analysis.
If any of these factors apply in your case, ask for a repeat PSA.
When a PSA Makes Good Sense
Early PSA testing makes the most sense if you fall into any of the following categories:
Family History: If you have a family history of prostate cancer, it’s advisable to begin PSA testing at 40 and repeat the test at six-month intervals.
African Americans: All African-Americans are advised to begin tests by age 40 regardless. The death rate from undiagnosed prostate cancer for African-Americans is currently two-and-a-half-times that for Caucasian men. This is partly for genetic reasons, and partly from reluctance to submit to a DRE—85% of cancers occur in the peripheral zone of the prostate gland, and therefore can be felt by the doctor performing the exam. A DRE is an essential diagnostic procedure.
Men Over 75: Nowadays, men over 75 are apt to be spared testing entirely. So you can always avoid the anxiety, and have a good time. On the other hand, you might just go for the PSA test anyway, and while you’re at it, have a thorough physical. I know a number of grateful men who never would have discovered that they had a serious heart problem or high blood pressure, if they hadn’t started with a PSA check. How long has it been since your last physical?
The Politics of PSA Testing
The best clinicians do not mindlessly screen all of their male patients. They decide which men should be tested based on age, symptoms, family history, expected longevity, general medical condition, physical examination findings, and—a significant factor—the patient's own request for the test. The goal of early detection remains to identify patients who have clinically significant cancers at a time when treatment is most likely to be effective.
Remember that, ultimately, the big decisions are all yours to make. Trust is crucial. So never hesitate to go for a second opinion. Bottom line, regardless of its shortcomings, the blood test for prostate-specific antigen is still the most useful and widely available method for detecting the presence prostate cancer. And if you want an encouraging statistic, here’s the really good news for men over fifty: 28 out of 30 of you who are reading this blog, and who do have prostate cancer, will die with it, not of it.
As you probably noticed, there is no “MD” after my name. Which means that my experience, my facts, and my emotional involvement are open to scrutiny and comment. In these blogs, I will be writing about matters that I know are of concern to men with prostate cancer, and to those who love them. You don’t need an MD after your name either, to point out something I’ve missed, or correct me if I’m off base. I welcome any PSA questions, advice or stories—reassuring or cautionary—that you’d care to share.
Article originally posted on April 12, 2011, on Prostate Snatchers: The Blog, by Ralph Blum
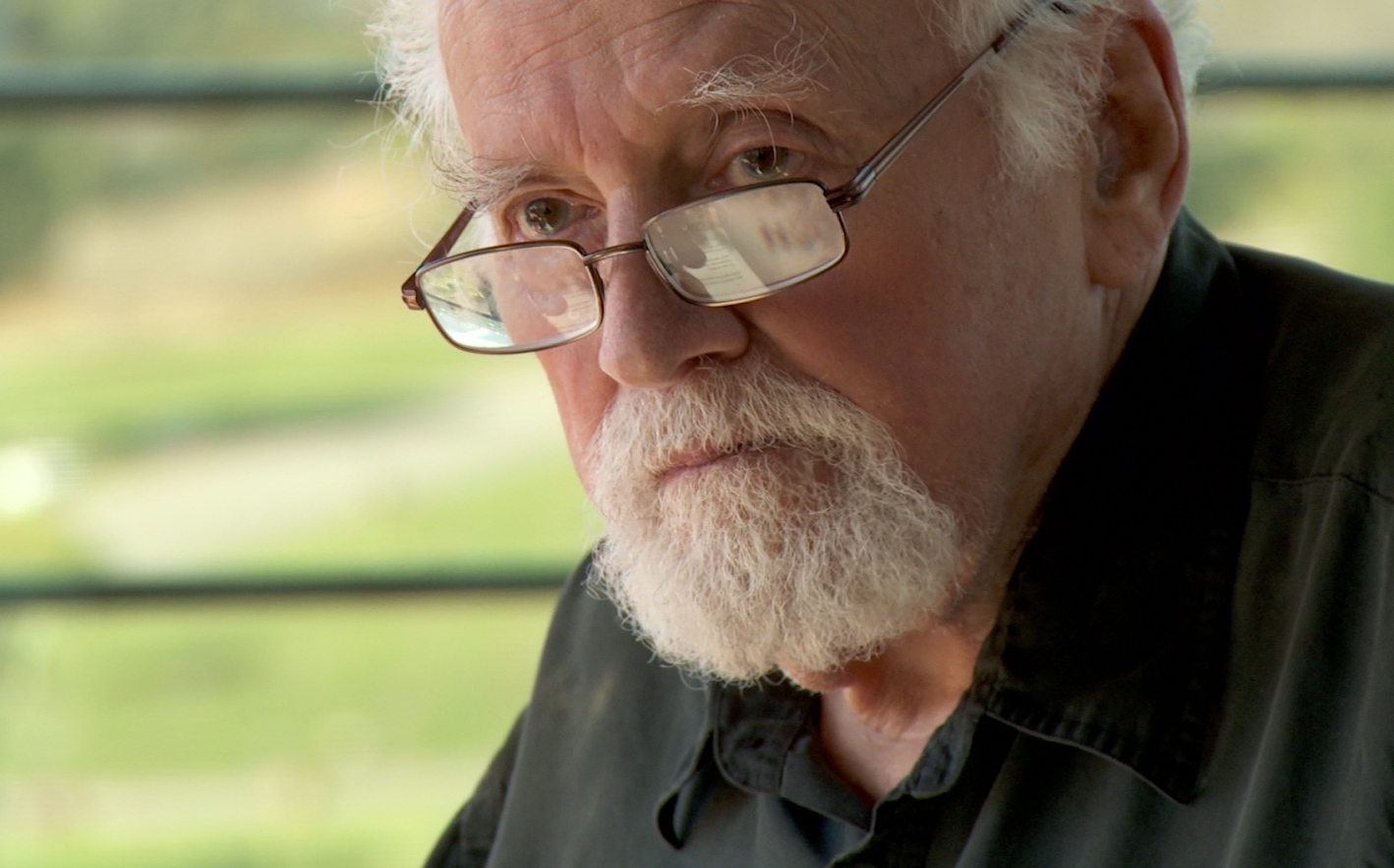
About Ralph Blum (1932-2016):
Ralph H. Blum was a cultural anthropologist and author, graduated Phi Beta Kappa from Harvard University with a degree in Russian Studies. His reporting from the Soviet Union, the first of its kind for The New Yorker (1961—1965), included two three-part series on Russian cultural life. He wrote for various magazines, among them Reader’s Digest, Cosmopolitan, and Vogue. Blum has published three novels and five nonfiction books. He lived with prostate cancer, without radical intervention, for twenty years.