Interpreting a Pathology Report: 15 Biopsy and Gleason Questions Answered by a Leading Pathologist
Prostate Insights | Volume 19. Issue 1
Jonathan Epstein, MD | Johns Hopkins University
Patients should personally review their pathology report. The report is an expert description of the information obtained from the needle biopsy. Typically, a copy of the report can be provided by the treating physician.
Although a urologist will typically be the person who presents the results of the biopsy to the patient, the official pathology report is generated by a pathologist—such as myself—a specialized physician with many years of training in the study and diagnosis of specimens removed by surgery or by needle biopsy.
The major components communicated in the report are the Gleason grade, which is a measure of how aggressive the tumor looks under the microscope, and the quantity of cancer. The quantity is judged two ways: The number of biopsy cores containing cancer (assuming, as is usually the case, that the biopsy was performed using standard random techniques). For example, if only 2 of 12 cores contain small amounts of cancer, the quantity of cancer (the presumed size of the tumor) would be small. At the other end of the spectrum consider the situation where 10 of the 12 cores contain cancer and each core is more than 50% replaced with cancer. In this case, the presumed size of the tumor would be large. So the quantity of the cancer within the prostate, as judged by the needle biopsy, is based both on how many cores contain cancer and the extent of the cancer replacing normal gland tissue within each single core.
The field of prostate pathology is immense and practically impossible to compress into a single article so to convey the basic elements of prostate pathology, the most efficient and concise approach is to address fifteen common questions I frequently encounter:
1. WHAT IS THE “GLEASON GRADE” OR “GLEASON SCORE?” WHAT DO THE NUMBERS IN THE GLEASON SCORE MEAN, FOR EXAMPLE, 3+4=7 OR 3+3=6?
The Gleason grading system assigns a pattern to the cancer cells depending on their appearance under the microscope, using numbers from 1 to 5. However, it is important to realize that in these modern times that patterns 1 and 2 are only used very rarely. Therefore, on a needle biopsy, the pathologist almost always reports the grade as pattern 3, 4 or 5. A higher number is assigned by the pathologist when the appearance of the cancer cells deviates more from visual appearance of normal prostate gland tissue. For example: If the cancerous tissue looks much like normal prostate tissue, it is pattern 1. If the cancer cells and their growth patterns look very abnormal, it is pattern 5. Patterns 2 through 4 have features in between these extremes.
Since prostate cancers in a single patient often have areas with different grades, the first pattern, when assigning a “score,” is the most common pattern seen after review of all the biopsy specimens, i.e., the pattern that makes up most of the cancer seen in the biopsy. The 2nd pattern that is assigned is the one showing the next most common pattern. These two different grades are then added together to yield the Gleason score (also called the Gleason grade). For example, if the Gleason score is written as “3+4=7”, it means most of the tumor is primarily pattern 3 and to a lesser amount pattern 4. These two numbers are then added together to create a Gleason score of 7. If the tumor has only one pattern throughout the whole tumor, the same pattern is counted twice in order to keep the grade in scale. For example, a biopsy core that is involved by only Gleason pattern 4 would have a Gleason score of 4+4=8.
2. WHAT DOES A GLEASON SCORE OF 6 MEAN?
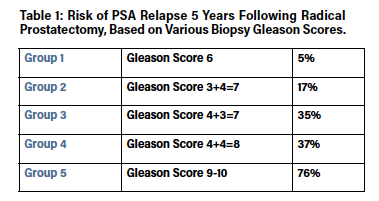
Gleason scores 2-5 tumors are very rare because they cannot be identified accurately on needle biopsy. So even though it is technically correct to say that the Gleason score can range from 2-10 suggesting that 6 would be “in the middle,” in actual practice, the Gleason score only ranges between 6 and 10. Therefore, a Gleason 6 actually represents the lowest grade (the most favorable) possible. Assigning the number 6 can lead to potential misinterpretation by patients. For example, Gleason score 6 cancer is almost always cured (see Table 1). Gleason score 6 cancers are so indolent that many men with these tumors are candidates for active surveillance. For this reason, I have proposed a modification of the Gleason score that more accurately transmits the favorable message about Gleason 6. On the other hand, most men with higher grade tumors will be recommended to undergo some type of treatment. Question #5 below expounds further on this proposal to revamp the way we report Gleason score. Full details of the proposal have been published in the medical journal called European Urology in September 2015.
3. What does it mean to have a Gleason score of 7?
A Gleason score of 7 can be made up of either 3+4=7 or 4+3=7, depending on whether the pattern 3 or pattern 4 is predominant. There is a big difference between these two grades. Table 1 shows the substantial difference in five-year cure rates. The biggest therapeutic difference between these grades is that more aggressive radiation therapy protocols are often given for Gleason score 4+3=7 and above.
4. What does it mean to have Gleason scores of 8-10?
Although Gleason score 8 cancers are aggressive, they are not as concerning as Gleason scores 9-10 tumors (Table 1). However, some patients with Gleason scores 9-10 can still be cured.
5. What is the best way to put all these different Gleason scores into a clinical context?
The best and simplest way to get a sense of what the Gleason score is predicting about the future behavior of the tumor, is by grouping them from 1 to 5 with group 1 having the best outlook and 5 having the worst. For example, Table 1 shows how these Gleason groupings predict cure rates with surgical treatment at a center of excellence. As can be seen, cure rates decline as the group number increases.
6. What does it mean when there are different biopsy cores with different Gleason scores?
Different cores may sample different areas of the same tumor, or the cores may sample different tumors in the prostate (it is fairly common for men to have more than one tumor). Because the grade may vary within the same tumor or between different tumors, different cores taken from the prostate may have different Gleason scores. The highest Gleason score observed in a particular patient is selected for predicting prognosis and deciding therapy.
7. Can the Gleason score from a random biopsy really tell what the cancer grade is in the entire prostate?
The Gleason score on biopsy usually reflects the cancer’s true grade. However, in about 20% of cases, the biopsy underestimates the true grade, resulting in under-grading. This can occur because randomly directed biopsy needles occasionally miss a higher grade (more aggressive) area of the cancer. Under-grading is statistically more likely to occur in men with: 1) larger tumors, 2) higher PSA levels, and 3) smaller prostates.
Somewhat less commonly, the true grade of the tumor is lower than what is seen on the biopsy, resulting in over-grading. For example, studies show that 16% of cases with a Gleason score of 3+4=7 on biopsy, will end up having Gleason score 6 when the surgically removed prostate is examined. Discrepancies between the biopsy Gleason and the final Gleason after surgery may be caused by inaccurate over-grading of the biopsy specimen by an inexperienced pathologist, or because the actual quantity of pattern 4 originally detected in the biopsy core turned out to be so small that it could not be found by the pathologist who examines the surgically removed prostate.
8. What does it mean if my biopsy report mentions special studies such as high molecular weight cytokeratin (HMWCK), ck903, ck5/6, p63, AMACR (racemase), 34BE12, or PIN4 cocktail?
These are special tests that the pathologist sometimes uses to help make the diagnosis of prostate cancer. Not all cases need these tests. Whether or not the report mentions these tests, there is no effect on the accuracy of the diagnosis.
9. What does it mean if my biopsy mentions that there is “perineural invasion”?
“Perineural invasion” means that cancer cells were seen surrounding or tracking along a nerve fiber within the prostate. When this is found on a biopsy, it means that there is a slightly higher chance that the cancer has spread along the nerves outside the prostate. Still, perineural invasion doesn’t necessarily mean that the cancer has spread outside the gland. Actually, other factors, such as the Gleason score and amount of cancer in the cores, are better indicators of cancer spread outside the gland. And even when tumor has microscopically spread out of the edge of the prostate, the majority of men are still cured.
10. What does it mean if, in addition to cancer, my biopsy report also says “high-grade prostatic intraepithelial neoplasia” or “high-grade PIN”?
“High-grade prostatic intraepithelial neoplasia” (or “high-grade PIN”) is a pre-cancer of the prostate. It has no importance whatsoever in someone who already has been diagnosed with cancer. In this case, the word “high-grade” refers to prostatic intraepithelial neoplasia and not the cancer, so it has nothing to do with the Gleason score or how aggressive the cancer is.
11. What does it mean if my biopsy report also says “atrophy” or “adenosis” or “atypical adenomatous hyperplasia” or “seminal vesicle?”
All of these terms are things that the pathologist sees under the microscope that are benign (not cancer). They are mentioned merely for completeness in the report because sometimes, to a physician with a less experienced eye, they might be misinterpreted as cancer. They are of no concern for the patient.
12. What does it mean if in addition to cancer my biopsy report also says “atypical glands” or “atypical small acinar proliferation (ASAP)” or “glandular atypia” or “atypical glandular proliferation?”
All these terms mean that the pathologist saw something under the microscope that suggests cancer may be present. However, the actual evidence for cancer is insufficient to be conclusive. Finding any of these is of no relevance to the overall outlook if cancer has already been diagnosed in another part of the biopsy.
13. How do pathologists measure the amount of cancer in the core?
There are multiple techniques used to quantify the amount of cancer found on needle biopsy. The most common are: (a) number of positive cores, (b) total millimeters of cancer amongst all cores, (c) percentage of each core occupied by cancer, and (d) total percent of cancer in the entire specimen. All of these different methods of measuring cancer volume on needle biopsy are tightly related with each other, such that it is difficult to demonstrate the superiority of one technique of measuring over the other. In general, a report which has the number of positive cores along with one of the other measurements is sufficient.
14. How can I be sure that the Gleason grade in the report is accurate?
Assigning the correct Gleason score is a skill just like any other that is developed through experience and practice. It is often prudent to have the biopsy material referred for a second opinion at a reference center to confirm the accuracy of the initial Gleason score that was assigned.
15. Does genetic testing with Prolaris and Oncotype provide additional useful information?
Preliminary studies seem to indicate that these tests can provide additional information about a cancer’s future behavior in a minority of patients who are tested. It is possible that these tests may also have some value in “cross checking” the accuracy of the Gleason score that has been assigned, though, at this time, testing for this purpose has yet to be evaluated in a clinical trial.
Concluding Thoughts
A few years ago, there was a news story about a polar bear attacking a man in Canada. Shockingly, the bystanders did nothing to help the poor man. Upon further review, however, it turned out that the reporter had neglected to report that the “bear” was only a cub, whose reach was lower than the man’s knees.
When facing a monstrous behemoth like “cancer,” the most important question to ask is “What kind of cancer am I dealing with?” With the currently available medical knowledge and technology, there can be no excuse for not knowing the exact grade of the cancer in order to make an informed treatment (or non-treatment) decision. Men facing a new diagnosis of prostate cancer should carefully scrutinize the pathology report and reflect carefully on its implications before rushing or being urged to make hasty treatment decisions.
Author Biography
Jonathan I. Epstein, MD, obtained a combined BA-MD degree from Boston University’s 6-Year Medical Program (1975–1981). Following his residency in anatomic pathology at The Johns Hopkins Hospital in Baltimore, Maryland and a fellowship in oncologic pathology at Memorial Sloan Kettering Cancer Center in New York, he joined the staff at The Johns Hopkins Hospital and has been there his entire career. At The Johns Hopkins Medical Institutions, he is Professor of Pathology, Urology, and Oncology; the recipient of the Reinhard Chair of Urological Pathology; and Director of Surgical Pathology. He is the past President of the International Society of Urological Pathology. Dr. Epstein has over 800 publications in peer-reviewed literature and has authored 51 book chapters. He is the author or coauthor of 7 books including “Interpretation of Prostate Biopsies” which is in its 5th edition. More recently, he authored or co-authored “The Gleason Grading System: A Complete Guide for Pathologists and Clinicians” and “Differential Diagnoses in Surgical Pathology: Genitourinary System.” Dr. Epstein has one of the largest surgical pathology consulting services in the world with approximately 12,000 cases per year, covering the full range of urologic pathology. He has lectured 349 times outside of his institution including 40 different countries.